Enhancing Recovery: Chronic Kidney Disease and Bedside Dialysis in Hospital Care
During National Kidney Month in March is the perfect time to talk about the prevalence of chronic kidney disease (CKD) in the United States. CKD develops gradually as the kidneys become damaged and work less effectively. Damaged kidneys may not filter and clean the blood as well as healthy ones, which can cause waste and fluid to accumulate in the bloodstream and other medical complications. These complications could include high blood pressure, heart disease, and stroke.
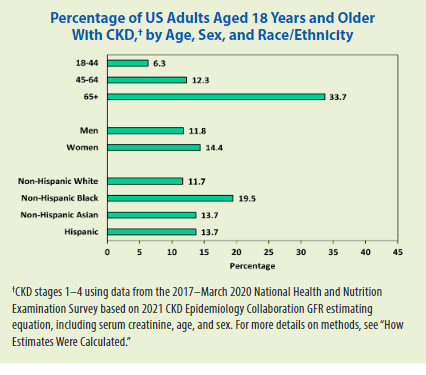
Adding to the seriousness of CKD is how many people are unaware they have it until symptoms progress. The Centers for Disease Control and Prevention estimates that as many as 9 of 10 adults who have CKD do not even realize it. Overall, CKD affects 1 in 7 US adults or about 35.5 million people.
Find a PAM Health Outpatient Center Near You
Source: https://www.cdc.gov/kidneydisease/publications-resources/ckd-national-facts.html
Risk Factors for Chronic Kidney Disease
One of the first steps in determining the risk for developing CKD is understanding the risk factors. As with many chronic conditions, there are multiple risk factors, both hereditary and non-hereditary, that can contribute to someone developing, including:
- Family history of CKD
- Inherited kidney disorders
- Previous kidney damage (including being injured in an accident)
- Obesity
- Being older than 65 years of age
- High blood sugar
- High blood pressure
Maintaining a healthy weight, eating a balanced diet, and exercising regularly can help manage blood sugar, weight, and blood pressure but cannot prevent all instances of CKD.
How Do You Know if You Have Chronic Kidney Disease?
With such large numbers of adults having Chronic Kidney Disease but not knowing it, it is important for individuals to talk to their physician if they have multiple risk factors. Their physician may talk to them about testing the blood for creatinine and urine for protein. If an individual has high levels of either, they may have Chronic Kidney Disease or an elevated risk. Certain medicines and lifestyle changes can slow the progression of Chronic Kidney Disease. The earlier CKD is detected, the more treatment options are available.
Did You Know?
According to the CDC, as many as 9 out of 10 adults who have chronic kidney disease don't realize it.

What Happens if CKD is Undiagnosed and Untreated?
There is no cure for CKD. When Chronic Kidney Disease advances without intervention (and sometimes even with it), end-stage kidney disease (ESKD) or kidney failure may occur. At this point, kidney damage is beyond repair through diet, exercise, or medications. Treatment options for ESKD include dialysis or a kidney transplant.
Types of Dialysis: Home, In-Center, and Peritoneal Dialysis
Dialysis is a medical treatment to help do what the kidneys no longer do effectively – filter the waste from the bloodstream. However, it is not a cure for kidney disease. The National Kidney Foundation categorizes the three main types of dialysis for ESKD as:
- Home dialysis
- In-center dialysis
- Peritoneal dialysis
While home dialysis has been shown to produce positive outcomes, it is not without risk. With the proper equipment, patients can perform dialysis in the comfort of their own home providing they have enough space for the equipment and have a trained dialysis partner present with them while they are on dialysis. This allows the individual to have easy access to treatment but requires specialized training and precautions to ensure the dialysis is done correctly and safely.
In-center dialysis is performed at a dedicated dialysis center. Individuals using this type of dialysis go to the same center/location on specific days and times to have trained medical professionals perform the procedure. Other people may also be getting dialysis at the same time. While some people appreciate having others around and form bonds with their fellow patients, other people may prefer more privacy.
The third type of dialysis, peritoneal dialysis, is an automated dialysis using the abdomen lining (peritoneum) to filter the blood. A few weeks after a surgeon has placed a catheter in the patient’s abdomen, the individual can then attach a bag filled with a special dialysis solution to filter the blood. Patients can cap the catheter and return to their normal activities for several hours before re-attaching the bag and allowing it to fill back up with the waste products. This process is repeated several times a day unless the patient is on automated peritoneal dialysis, which is a special machine (cycler) that performs dialysis while the patient is asleep.
Types of Outpatient Dialysis
Home Dialysis
- Patient self-administers dialysis
- Involves specialized equipment and space for it in home
- Requires trained dialysis partner to be present during treatment
- Shown to product positive outcomes with benefit of patient being in comfort of their home
- Involves some risk if not done correctly or safely
In-Center Dialysis
- Performed at a dedicated dialysis center by trained medical professionals
- Patient visits designated center on a set schedule
- Not private; multiple patients can be receiving dialysis in the same space at the same time
Peritoneal Dialysis
- Form of dialysis that uses the abdomen lining, the peritoneum, to filter the blood
- A catheter is surgically placed in the peritoneum, allowing necessary access for dialysis
- Repeated several times daily
- Some patients are on automated peritoneal dialysis, in which a machine performs it during sleep
In-Hospital Dialysis: Bringing Treatment to the Bedside
For dialysis patients who find themselves facing a hospital stay, bedside dialysis can be a lifeline. This on-site treatment modality offers numerous advantages, particularly for critically ill or immobile individuals who may not be able to undergo traditional dialysis in a specialized unit and who cannot leave the hospital to go to a dialysis center. Most PAM Health specialty care hospitals and inpatient rehabilitation hospitals offer bedside dialysis services by specially trained nurses.
By bringing dialysis directly to the patient's bedside, healthcare providers like PAM Health can minimize the logistical challenges associated with transportation and transfer, ensuring timely and uninterrupted access to essential care. This not only enhances patient comfort and convenience but also reduces the risk of complications and improves treatment adherence.
Moreover, bedside dialysis facilitates seamless integration with other aspects of patient care, including scheduling therapy sessions and other appointments so they do not conflict with the dialysis schedule. By enabling interdisciplinary collaboration and coordination, the hospital team ensures that dialysis therapy is seamlessly incorporated into the broader care plan, addressing the patient's unique medical, nutritional, and psychosocial needs.
Furthermore, the provision of comprehensive renal care within the hospital setting fosters continuity and coherence across the care continuum. As patients transition from acute care to rehabilitation and beyond, seamless coordination ensures that their kidney health remains a priority, facilitating a smoother recovery trajectory and reducing the likelihood of readmissions.

Find A PAM Health Location Near You
Find a location near you to receive personalized care for your chronic kidney disease.
Find A LocationNavigating the Journey with Chronic Kidney Disease
In conclusion, the first step to battling kidney disease is understanding what it is, the risk factors, and treatment options. Individuals should talk to their physician about their personal situations to determine if testing is needed. If CKD is diagnosed, physicians can work with the patient to develop a plan of care to control and slow the progression of the disease. If ESKD develops, patients should talk to their medical provider about which dialysis option is best for their situation. Finally, if a dialysis patient ever requires an extended hospital stay to recover from illness or injury, finding a hospital that provides bedside dialysis can help with their overall recovery. Kidney rehabilitation and bedside dialysis play indispensable roles in optimizing patient outcomes and promoting recovery within the hospital setting. These interventions not only address the immediate needs of patients with renal issues but also empower them to actively participate in their care journey.
By embracing a comprehensive approach that encompasses education, support, and interdisciplinary collaboration, healthcare providers can make a meaningful impact on the lives of individuals grappling with kidney disease. As PAM Health strives for excellence in patient care, the integration of kidney rehabilitation and bedside dialysis stands as a testament to our commitment to holistic, patient-centered healthcare delivery.
Looking for dialysis services? Click here to find a PAM Health location near you.