
Parkinson’s disease is a nervous system disorder that affects over 1 million Americans. This disease involves the part of the brain that controls movement. The main symptoms include tremors, muscle rigidity and difficulty with coordination, balance and walking.
Although there is no cure for Parkinson’s disease, various treatments can relieve symptoms and help patients maintain their quality of life. Physical therapy is one form of treatment known to help individuals with Parkinson’s disease increase mobility, strengthen their muscles, improve coordination and balance, and ultimately, remain independent. This post explores the different types of physical therapy and how to make the most of a rehabilitation program.
Explore Physical Therapy Services Offered by PAM Health
What Is Physical Therapy?
Physical therapy is a specialized form of health care that involves evaluating and treating a person with limited mobility. It is used to treat many conditions, including arthritis, amputations, injuries and Parkinson’s disease. Physical therapists are licensed professionals trained to apply individualized techniques to help patients regain mobility.
How Can Physical Therapy Help Parkinson’s Disease?
Physical therapy is an important part of a treatment plan for Parkinson’s disease. It aims to help individuals with Parkinson’s disease remain active and independent as long as possible. According to a recent meta-analysis, physical therapy significantly improves symptoms related to motor skills. The Parkinson’s Foundation states that increasing physical activity to 2.5 hours a week or more can help people with Parkinson’s disease maintain their quality of life.
Overall, physical therapy can help with the following:
- Increasing endurance
- Strengthening muscles
- Reducing muscle stiffness
- Improving gait
- Reducing freezing episodes
- Improving balance and coordination
- Increasing flexibility
- Improving posture
- Decreasing falls
- Reducing pain
Because physical therapy improves motor skills and decreases pain, you can expect it to help with many of your regular activities, such as getting up from a chair, climbing stairs and getting into and out of a car.
Physical therapy can also improve other symptoms associated with Parkinson’s disease, such as depression, anxiety and fatigue. Lastly, it can help with other health issues that impair mobility, like joint pain.
Doctors recommend beginning an evidence-based physical therapy program as soon as possible. Exercise can induce neuroplasticity, or the brain’s ability to change in response to behavioral changes. When you begin physical therapy, your brain learns new ways to move and think. Exercise also helps brain cells stay healthy. In other words, physical therapy may slow the progression of Parkinson’s disease.
Even if you are at a later stage of the disease, it is still worth starting a physical therapy program. Physical therapy can improve symptoms for patients at any stage of Parkinson’s disease.
Common Physical Therapy Goals
As a physical therapy patient, you will work with a physical therapist to set and achieve realistic goals. A physical therapist will create a tailored, research-based exercise routine for you. They will first evaluate your current abilities and consider the areas you want to improve. The therapist will then design an exercise program to target those areas. Typically, physical therapy involves small achievements that build to a bigger goal.
Although your physical therapist will create an exercise plan based on your unique needs, shared goals for patients with Parkinson’s disease include:
- Learning about exercises: Physical therapists teach patients about various exercise types to empower them and help them manage the disease independently. They show patients how to recognize and react to new symptoms using physical activity. Physical therapists also teach patients how to exercise safely.
- Improving movement: Changes in walking, balance and posture are common symptoms of Parkinson’s disease. Your physical therapist will assess your mobility and posture and design strategies to help you move better and stay active.
- Addressing fall risk: Due to motor symptoms, people with Parkinson’s disease are at a high risk of falling. Falls can lead to injuries and the fear of falling, impacting a person’s ability to maintain independence. Your physical therapist will evaluate your fall risk and choose exercises that will help prevent falls.
- Treating pain: Your physical therapist will evaluate any muscle or joint pain you are experiencing that interferes with your daily activities. They will set exercise goals to help you complete everyday tasks with less pain.
Types of Physical Therapy for Parkinson’s Disease
The type of therapy you receive for Parkinson’s disease depends on your symptoms, needs and what you wish to achieve. Common therapy options for Parkinson’s disease management include:
Amplitude Training
Amplitude training is a physical therapy strategy designed to reduce bradykinesia and hypokinesia. Bradykinesia is a slowness of movement and one of the main symptoms of Parkinson’s disease. Hypokinesia refers to small movements and is another common symptom of Parkinson’s disease.
With amplitude training, patients practice making exaggerated movements, such as swinging their arms or taking high steps. This therapy form helps retrain your muscles and prevent you from taking small, slow movements.
Reciprocal Movements
Reciprocal movements happen at the same time in opposite directions. For example, swinging your arms as you walk is a reciprocal movement. Parkinson’s disease may impair a person’s ability to make reciprocal movements which can cause balance issues, but physical therapy can help.
Your physical therapist might have you use a stationary bike or elliptical machine to strengthen reciprocal patterns. They may also recommend that you practice reciprocal movements on your own by focusing on swinging your arms as your walk. Dancing and tai chi can also improve your ability to move.
Balance Training
Your brain uses input from your eyes, ears, muscles and joints to keep your body balanced. Parkinson’s disease might affect your balance system and make it challenging to stay steady as you walk. If you are struggling with balance, your physical therapist can incorporate balance training in your exercise plan and teach you techniques you can use at home. Balance training is typically an essential part of Parkinson’s disease treatment because it improves gait and helps prevent falls.
Stretching
Stretching improves flexibility and reduces the muscle stiffness associated with Parkinson’s disease. Being flexible is essential for everyday movements like walking, bending and lifting. When you increase flexibility through stretching exercises, you may have an easier time getting out of bed, putting on clothes, picking items off the floor and completing various other tasks. You can tell your physical therapist whatever area you want to improve regarding flexibility, and they will show you stretches to target those muscles.
Muscles that move joints are the ones that typically tighten with Parkinson’s disease. For this reason, the Parkinson’s Foundation recommends a stretching routine that focuses on these areas:
- Shoulders and elbows
- Calves
- Hamstrings and knees
- Wrists and palms
- Lower back
- Neck
- Chest wall
You can practice the stretches your physical therapist teaches you frequently throughout the day to reduce muscle stiffness.
Strength Training
Muscle strength is vital to staying active and maintaining independence. Parkinson’s disease and aging can both lead to muscle weakness without a strength training routine. In general, people strengthen their muscles by lifting weights or using weight machines. People can also use resistance bands or their own body weight to build up their muscles. No matter what stage of Parkinson’s disease you are in, you can still make your muscles stronger.
Your physical therapist will choose strength training exercises that are safe for you and will improve problem areas. Your physical therapist may recommend strengthening the following muscles to help with your posture, increase endurance and improve motor symptoms:
- Back muscles
- Buttocks
- Thigh muscles
- Core muscles
- Triceps
Talk to your physical therapist about your most important goals so they can help you in the way you need. For example, if you have difficulty getting up from a chair, your physical therapist might help you build muscles in your legs.
Dual-Task Practice
Parkinson’s disease can make it challenging to multitask or switch from one task to the next, increasing fall risk and making everyday activities more difficult. If you have trouble doing more than one task at a time, your physical therapist might have you practice two activities simultaneously to help with this symptom. For example, they might ask you to try walking while counting, bouncing a ball or naming objects. The point is to retrain your brain to do two things at once. Dual-task practice can also enhance balance skills.
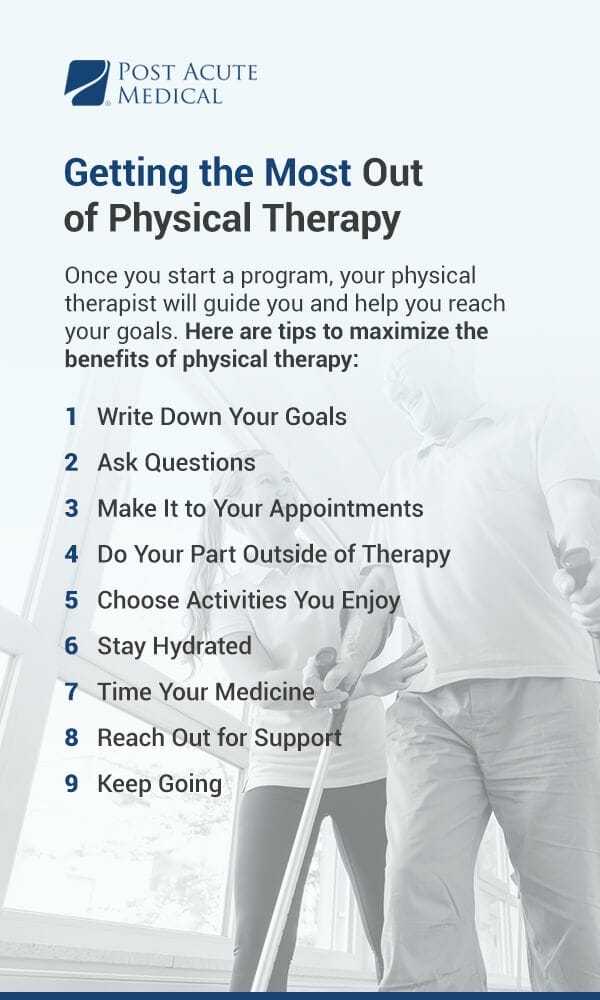
Getting the Most Out of Physical Therapy
Physical therapy will teach you the right exercises to target the symptoms you want to make better. Exercise is crucial for improving Parkinson’s disease symptoms and maintaining general health. Even if you do not have mobility or pain issues, start an exercise program as soon as possible to delay the disease’s progression.
Once you start a program, your physical therapist will guide you and help you reach your goals. Still, it is in your power to make the most of your treatment. Here are tips to maximize the benefits of physical therapy:
Write Down Your Goals
Before you meet with a physical therapist, write down all the goals you want to accomplish. Writing your goals can help you organize your thoughts and focus on what is most important to you. When listing your goals, consider the areas you are struggling with and would like to improve most. Your goals will provide direction for your treatment and help you stay motivated. You can adjust your goals or create new ones as needed.
Ask Questions
Jot down a list of questions to ask a physical therapist before you begin a program. For example, you might ask a physical therapist if they have experience treating people with Parkinson’s disease. Other questions you might ask include:
- What should I wear to appointments?
- Does my insurance cover the program?
- What is your cancellation policy?
- What can I expect to happen during my first appointment?
If you have questions or concerns during therapy, feel free to ask. Your physical therapist should encourage you to ask questions and make you feel comfortable discussing any concerns.
Make It to Your Appointments
The number of physical therapy appointments you need depends on your condition and goals. Generally, your first appointment will include an evaluation and exercise recommendations. In following appointments, your physical therapist will check your progress and add or modify exercises according to your needs. Make sure you attend all of your appointments to stay on track.
Do Your Part Outside of Therapy
It is vital to practice the exercises you learn in physical therapy at home. Doing exercises at home will help you reap the most benefits from physical therapy and keep you strong. Your physical therapist will show you activities that are safe for you to do outside of therapy sessions.
In addition to doing planned exercises, consider ways to increase general physical activity. For example, doing housework, gardening or walking around a store are ways to increase physical activity every day.
Choose Activities You Enjoy
Make sure you choose exercises that are fun and challenging but not too difficult. For example, if you enjoy walking in nature, make that part of your exercise routine. It is important to enjoy appointments with your physical therapist, too. If your physical therapy program is not working for you, talk with your physical therapist so they can change your routine.
If you choose activities you like, you are more likely to stick to your plan and reach your goals.
Stay Hydrated
Make sure you stay hydrated so you can be safe and feel good as you exercise. In general, aim to drink at least eight cups of water each day in addition to any other beverages you might have. If you are concerned about using the bathroom too much, try to consume most of your day’s fluids in the morning and afternoon so that you can rest better at night. It may also help to plan bathroom breaks at specific times so you can go before it becomes urgent.
Time Your Medicine
The International Parkinson and Movement Disorder Society recommends patients exercise during “on” periods whenever possible. Your “on” time is when your medications are most effective. Exercising when your medicine works best can help prevent falls.
Reach Out for Support
It can be challenging living with Parkinson’s disease, but you do not have to manage the symptoms alone. If you find yourself feeling discouraged or frustrated, share your feelings with others. Spend time with supportive friends and family members, or consider joining a support group. You might also speak with a counselor to address depression, anxiety or any other mental health issues you experience. By taking care of your mental and emotional health, you will be better positioned to reach your physical health goals.
Keep Going
Exercise is an integral part of a healthy lifestyle for all individuals. For physical activity to have the most significant impact, you need to exercise consistently long-term. By doing so, you will feel stronger, healthier and happier.
To help you stay motivated, here are a few suggestions:
- Choose fun activities
- Exercise with a friend
- Try new exercises once in a while
- Schedule exercise into your day and treat it as an important appointment
- Take an exercise class in something that interests you
If you choose activities you love, you will be glad exercise is a part of your life.

Find a Post Acute Medical Center Near You
Parkinson’s disease is a complex disorder that affects every person differently. If you or a loved one have Parkinson’s disease, you can still enjoy life and engage in fun activities. An individualized physical therapy program can help keep you on your feet and enhance your overall well-being.
At Post Acute Medical, our compassionate physical therapists are trained to help individuals with Parkinson’s disease improve their symptoms and reach their goals. To learn more about our comprehensive Parkinson’s disease rehabilitation program, contact a Post Acute Medical facility near you.


