
Uncomfortable and even painful swelling can occur in the body for many reasons, including lymphedema. Primary lymphedema is a relatively rare condition, affecting 1 in 100,000 people, while secondary lymphedema is more common. One in 1,000 people in the U.S. will experience secondary lymphedema.
How does this disease develop? What are the risk factors? The answers to these questions are different depending on the type of lymphedema — primary or secondary. Learn about both types of the disease below and how to manage the condition.
Find a Lymphedema Specialist Near You
What Is Lymphedema?
Lymphedema is a chronic condition that causes swelling in the body. It most commonly occurs in the arms and legs, but it can happen anywhere in the body, including the hands, chest, neck, face, and genitals. A collection of excess lymph fluid causes swelling.
Lymph fluid is a vital part of the lymphatic system, which also includes lymph nodes, lymphatic vessels, adenoids, tonsils, thymus, and the spleen. The lymphatic system moves lymph fluid, which contains white blood cells, throughout the body. This process helps remove toxins and waste from the body, making the lymphatic system part of our immune system.
Lymphedema occurs when the lymphatic system is unable to drain lymph due to damage or a blockage. Without draining, this high-protein fluid builds up and causes the swelling associated with lymphedema.
Certain conditions can increase the risk of developing lymphedema. Obesity and older age are considered risk factors for lymphedema. Additionally, certain types of arthritis are associated with a higher risk of lymphedema.
Symptoms of Lymphedema
Lymphedema is most easily recognized by visible swelling. However, swelling, particularly in the early stages of the condition, may be difficult to spot. If the arm changes even just two centimeters in diameter, this could suggest the development of lymphedema. If you know you are at risk of developing lymphedema, take note if an item of clothing that previously fit well feels tight on your arms or legs.
You may experience other symptoms of this condition before you can see swelling. You can experience swelling, along with other symptoms, in varying levels of severity throughout your entire experience with the condition.
In addition to swelling, symptoms of lymphedema include:
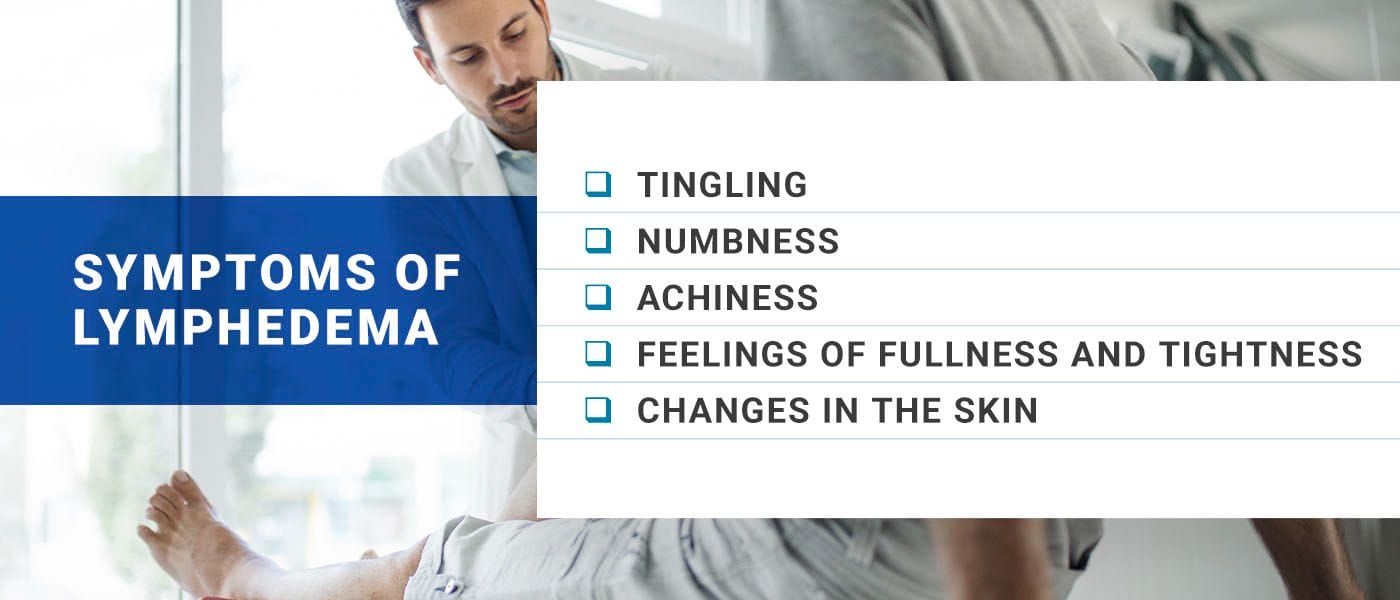
- Tingling: A tingling sensation in the affected area of the body could indicate lymphedema. You may feel this in the arms, underarms, hands, breasts, or chest. This sensation can sometimes be described as “pins and needles” or as a sensation of increased warmth. People with lymphedema may also experience shooting pains in different areas of the body.
- Numbness: You may experience numbness in the affected areas of your body, whether it is in the limbs or elsewhere. The feeling may come and go.
- Achiness: Lymphedema can cause flu-like symptoms, such as body aches. You may also experience feelings of tenderness in the affected areas and develop a fever.
- Feelings of fullness and tightness: The swelling caused by lymphedema may be accompanied by feelings of fullness or tightness. You might feel like you have less flexibility in the joints of the affected limbs.
- Changes in the skin: Lymphedema can also affect the skin. You may notice puffiness, red areas, or a rash. Hardening, itching, and pain are also common symptoms.
Swelling from lymphedema may develop slowly or come on suddenly. Your symptoms can help your doctor make a formal lymphedema diagnosis, but they may order tests to understand the cause of the condition. Imaging tests like an MRI scan, CT scan, and Doppler ultrasound can provide a visual of the lymphatic system and pinpoint any blockages responsible for the fluid buildup.
Get Help for Your Lymphedema Symptoms
Causes of Lymphedema
Various factors, including genetic conditions, infection, and cancer treatment, can cause lymphedema. Primary and secondary lymphedema can differ in terms of causes and risk factors. The main differences between the two include:
Primary Lymphedema
Primary lymphedema results from hereditary or genetic anomalies that cause the lymphatic system to not develop correctly. More specifically, aplasia refers to when organs and limbs do not develop and causes the lymph nodes to also never form, hypoplasia occurs when parts of the lymphatic system are underdeveloped, and hyperplasia refers to when lymph collectors are larger than normal. All three can lead to lymphedema, though they can also impact other areas of the body or be caused by other conditions.
The three main types of primary lymphedema include:
- Lymphedema praecox: Also referred to as Meige disease, lymphedema praecox is the most common type of primary lymphedema. The congenital condition does not cause obvious symptoms until puberty or later. Swelling typically starts at the feet and gradually travels upward.
- Congenital lymphedema: Also known as Milroy’s disease, this form of primary lymphedema is present at birth due to genetic factors. It can be associated with other genetic conditions, such as Turner syndrome.
- Lymphedema tarda: Lymphedema tarda is a condition that develops later in life. People with this condition may not experience symptoms until age 35 or after.
Secondary Lymphedema
Secondary lymphedema is acquired, meaning another disease or outside factor causes it. Some of the potential causes of secondary lymphedema include:
- Cancer: Cancer can disrupt the lymphatic system and cause lymphedema. When a tumor grows, it can put pressure on lymph vessels, making it more difficult for lymph fluid to flow through them. Cancer cells can also block the flow of lymph. Breast cancer is commonly associated with secondary lymphedema.
- Cancer treatment: Cancer treatment can also cause secondary lymphedema. In some cases, cancer patients need to have the lymph nodes in their underarms removed to prevent the spread of cancer. Lymph node removal is associated with an increased risk of developing secondary lymphedema. Radiation therapy, particularly when directed at the chest and underarms, can also increase the risk.
- Surgery: Surgery on the chest, such as surgery to address breast cancer, can also lead to secondary lymphedema. Scar formation following surgery can also affect the lymphatic system.
- Infection: Infection following surgery could increase the risk of secondary lymphedema. Infection at the incision site can cause inflammation and stress to the lymphatic system as it tries to handle increased blood and fluid flow.
- Trauma: The lymphatic system rests less than half an inch beneath the surface of the skin. Traumatic injuries, such as the crushing of a limb or severe burns, can damage the lymphatic system and increase the risk of secondary lymphedema.
- Parasites: Lymphatic filariasis is a type of disease caused by a parasite. The parasite, Wuchereria bancrofti, is transmitted via mosquito bite. Once inside the body, the worms live in the lymph system. This type of secondary lymphedema is considered a neglected tropical disease.
- Other health conditions: Conditions that affect other organs in the body can contribute to the development of secondary lymphedema. Kidney failure, for example, affects the body’s ability to remove excess fluid. If fluid builds up in the body, it can stress the lymphatic system and increase the chances of lymphedema. Conditions affecting the heart and vascular system can also decrease the body’s ability to move fluid throughout the body, leading to stress on the lymphatic system.
Risk Factors for Lymphedema
Other risk factors for primary and secondary lymphedema include:
- Obesity: People with obesity can have excess fat or adipose tissue that places pressure on vessels and lymph nodes. The extra pressure may impact how well your lymphatics system can drain lymph.
- Blood vessel issues: Blood vessels carry between 80% and 90% of fluid throughout our bodies. Any issue that impacts our blood vessels or vascular system can lead to chronic blood vessel problems, sometimes resulting in lymphedema.
- Heart conditions: People with heart problems, specifically congestive heart failure, can develop lymphedema. The lymphatic ducts empty lymph back into the heart. When the heart is not functioning as it should, you might notice weight gain or swelling in the legs.
- Lack of physical activity: When you move your legs, the muscles boost lymphatic circulation. Those who are not active can experience swelling in the legs.
Can Lymphedema Be Cured?
Lymphedema is a chronic condition that cannot be cured at this time. It is possible to reverse the effects of mild lymphedema, or stage 1, but the risk for the return or worsening of symptoms is still possible. Right now, treatment focuses on managing symptoms to improve quality of life.
Early detection is key in treating lymphedema. If this condition is left untreated, the severe swelling it causes can lead to permanent changes to the body’s tissue. If you know you are at risk for developing lymphedema, there are some steps you can take to watch for symptoms. You can engage in self-lymphatic massage to help promote proper drainage, for instance.
Following cancer treatment and surgery, you can take steps to help prevent secondary lymphedema, including:
- Protecting your limbs: Take extra steps to protect the arms or legs targeted by radiation or affected by surgery. Try to avoid getting small cuts or scrapes on those limbs, and avoid wearing tight clothing that could constrict those limbs.
- Skincare: A thorough skincare routine can help you recognize any subtle changes to your skin, and keeping the skin clean can reduce the risk of infection.
- Elevation: Elevate your affected limbs if possible. For example, you can rest your arm above the level of your heart while you are sitting and relaxing in the evening.
You can also watch for any of the symptoms associated with the condition, even mild swelling, and talk to your doctor immediately. Monitoring and early detection can help prevent lymphedema from becoming more serious. Ask your doctor if they have experience treating lymphedema or search for a provider who does. Lymphedema can sometimes be difficult to diagnose, and not all providers specialize in treating this condition.
Lymphedema symptoms can come and go. Some people need continuous treatment, while others may only require treatment when symptoms flare up.

Lymphedema Treatment and Management
Although primary and secondary lymphedema are chronic conditions, several treatment approaches can help you manage your symptoms, including:
- Compression: Compression is one of the frontline treatments for managing the swelling caused by lymphedema. Lymphedema therapists can teach you how to wrap bandages around the affected area of the body to help move the excess fluid. Treatment may also involve wearing compression garments. You may use the garments by themselves or attach them to a device that can apply additional pressure to promote movement of the fluid.
- Massage: Manual lymphatic drainage is a massage technique that helps move the fluid from the affected area of the body to other body parts with working lymph vessels. The massage is a gentle treatment your therapist can perform. Your therapist can also teach you how to do the technique at home.
- Exercise: Gentle forms of exercise can help promote fluid drainage in the affected areas. Your therapist can teach you how to do these exercises on your own. They may recommend activities like swimming, walking, or yoga to stimulate lymph flow.
- Complete decongestive therapy (CDT): CDT is an integrative approach to lymphedema treatment. It combines manual lymphatic drainage, compression therapy, different types of exercise, and skincare. The first phase of this treatment approach focuses on decongestion, while the second is targeted at maintenance. Those with a history of blood clots, heart failure, high blood pressure, or diabetes might not be recommended CDT.
- Surgery: Surgery may be suggested in more severe cases of lymphedema. Lymphatic bypass involves connecting lymphatic vessels to direct fluid away from obstructions and encourage proper draining. Healthy, functioning lymph nodes can also be transferred from other parts of the body to the affected areas.
Tips for Living With Lymphedema
Living with lymphedema requires a comprehensive approach, including lifestyle changes and emotional support. You may experience a range of feelings, and it can be uncomfortable to get around when your leg or arm is swollen. Know that you are not alone, and in time, you can learn how to manage your symptoms to improve your quality of life. Here are some tips:
Wear Loose-Fitting Clothes
You can make a few changes to your wardrobe, such as avoiding tight-fitting socks, tights, pants, and shoes. Make sure any jewelry does not squeeze your arm.
Sit Properly
When sitting, keep your feet flat on the floor. Avoid crossing your legs to keep fluid moving in your legs. If you work an office job or sit for most of the day, remind yourself to take plenty of breaks to get up and move around. You might even put your leg on a stool or chair or lie down for a few minutes. If you have swelling in your arm, prop it up on a cushion to keep it raised at a comfortable level, but avoid lifting it above your shoulders for too long.
Travel Safely
If you have a flight in the near future, ask your doctor about wearing compression garments on your affected limbs. Many recommend wearing the bandaging before air travel and for a few hours after arriving at your destination to stay comfortable.
Join a Support Group
Being diagnosed with a chronic condition can feel disheartening, and you may experience various emotions, from sadness to stress. But know that you are not alone. By caring for your mental health, you can start to feel better and improve your overall outlook. Joining a support group can offer valuable information, encouragement and a sense of belonging. Sharing your experiences with others can be incredibly comforting.
Take Care of Your Skin
When living with lymphedema, be sure to keep your skin clean, protected, and moisturized. The condition puts stress on the skin, making it more prone to infection from cuts, scrapes, and scratches, and infections can lead to complications. Try the following to protect your skin:
- Wash your hands: Use soap and warm water to wash your hands and keep them clean throughout the day. Be sure to clean them after going to the bathroom or touching dirty linens or surfaces.
- Moisturize: Moisturize your skin daily to prevent cracks and scrapes. An unscented lotion can do wonders in hydrating your skin, keeping it smooth and restoring its natural barrier.
- Protect your skin outdoors: When outside, be sure to wear insect repellant to avoid bug bites that could cause you to scratch your skin. Wear sunscreen to avoid sunburn.
- Treat injuries immediately: Even minor cuts can lead to infections. If you notice a scratch or crack, wash the injury with soap and water, apply antibiotic ointment and cover it with a bandage. Call your health care provider if you notice signs of an infection, such as redness, fever or increased swelling.
Hydrate and Eat a Balanced Diet
Stick to a balanced diet rich in fruits, vegetables and lean proteins to maintain a healthy weight and reduce pressure on the lymphatic system. Staying hydrated is also critical to maintaining normal fluid movement throughout the body.
Talk to a Mental Health Professional
Living with any type of chronic condition can be emotionally challenging. Do not hesitate to seek support from a mental health professional if you are struggling. Counseling can offer various coping strategies for the emotional aspects of this condition. You can also try stress management techniques like deep breathing or meditation, and be sure to get plenty of rest and relaxation.
Monitor Your Symptoms
Track any changes in your symptoms, such as increased swelling, pain, or skin changes. This information can help your health care provider adjust your treatment plan as needed.
Increase Awareness and Advocacy
Educate yourself and those around you about lymphedema. The more you know about the condition, the more you can care for yourself. The more others know about lymphedema, the more understanding and support you will likely receive. Advocate for yourself and be proactive in seeking the best care for this condition available.
PAM Health’s Lymphedema Management Program

Whether you suffer from primary or secondary lymphedema, we can help. Post Acute Medical’s Lymphedema Management Program focuses on addressing your symptoms to improve your quality of life. Here is what you can expect from a treatment plan developed through our program:
- Drainage: Our providers are trained in manual massage techniques to promote the drainage of excess fluid causing swelling.
- Compression therapy: Compression therapy involves wrapping the affected limb to direct the flow of fluid away from that part of the body. Our providers can show you the proper wrapping technique.
- Exercise: Regular exercise can help to improve lymph drainage. Our providers will work with you to establish an exercise regimen to help you stay fit and improve your range of motion.
- Education: Lymphedema is a chronic condition, which means you need to find the treatment that works best for you. Our team provides education about your different options to help you learn about the approaches and lifestyle changes that work for you.
We also work closely with you to provide support for the psychological impact of lymphedema. The effects on your physical appearance and the pain caused by the disease can be significant. We help you to develop coping skills and improve your self-esteem.
Find a Location for Personalized Lymphedema Care
Find a PAM Health Location Near You
Lymphedema is a chronic condition that can have a serious impact on your quality of life. Treatment can help you to manage the condition and alleviate your symptoms. Post Acute Medical has several hospitals specializing in this condition, including:
- PAM Rehabilitation Hospital of Allen
- PAM Rehabilitation Hospital of Clear Lake
- PAM Rehabilitation Hospital of Round Rock
- PAM Rehabilitation Hospital of Victoria
- PAM Specialty and Rehabilitation Hospital of New Braunfels
- PAM Specialty Hospital of Covington
- PAM Specialty Hospital of Lufkin
- PAM Specialty Hospital of Hammond
- PAM Specialty Hospital of San Antonio
- PAM Specialty Hospital of Tulsa
- PAM Specialty Hospital of Wilkes-Barre
- Rehabilitation Hospital of Overland Park
- Warm Springs Rehabilitation Hospital of Thousand Oaks
Find a location near you to start treating your condition and receive the support you need to improve your quality of life.
Find a PAM Health Location Near You



